Cart
Sub-Total: $0.00
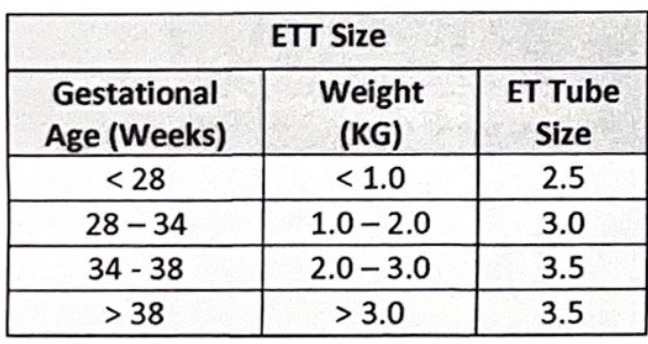
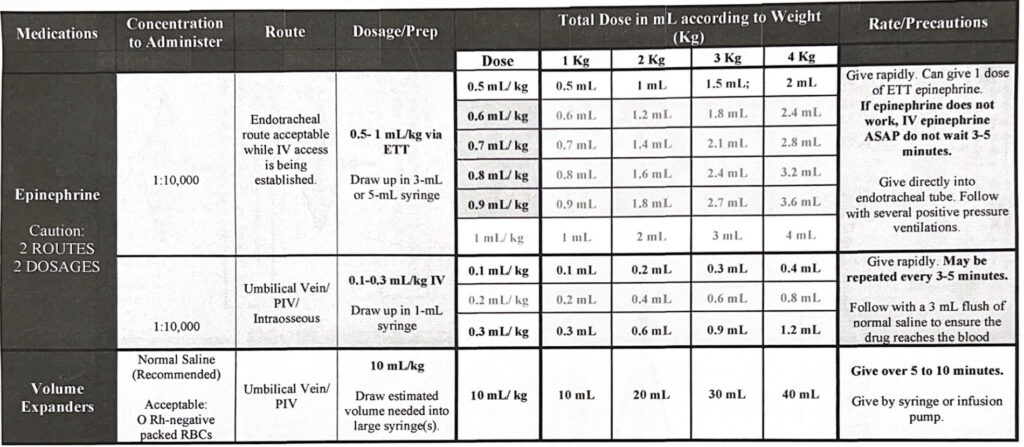
Preparation is key! All the resuscitation equipment checklists will be included in the NRP textbook. It is our job as NRP providers to be able to prepare the proper equipment needed to assist an apneic infant or neonates requiring chest compressions and epinephrine. Most of all of our equipment will be located in the drawer of the warmer or close to the warmer. All steps of resuscitation must be performed quickly and efficiently. Be familiar with where your facility keeps its equipment and we will be demonstrating how to use the equipment in our skills session.